Addiction research
ADDICTION RESEARCH: BELIEVING IN THE FUTURE1In global terms, alcohol research has been a growth industry in recent decades, as TomBabor has recently documented, and I believe the same could be documented for illicit drugs, forpsychopharmaceuticals, and for tobacco research. There is some reason to believe that the periodof growth may be coming to an end. The growth has, in any case, been highly
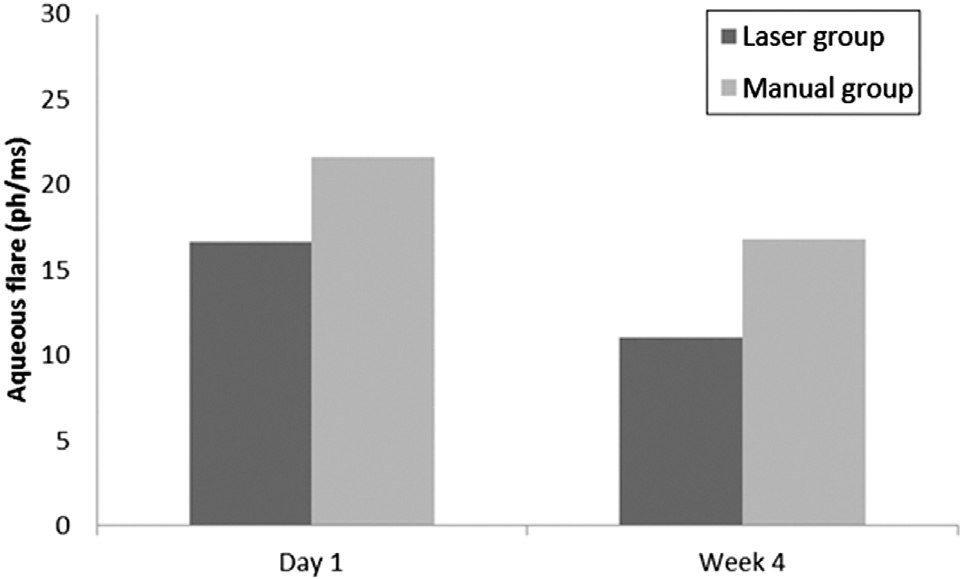 ANTERIOR CHAMBER FLARE AFTER LASER-ASSISTED CATARACT SURGERY
salt solution (BSS Plus) fluid volume used during surgery, in-terval between the laser procedure and initiation of manualsurgery steps, postoperative IOP, and the change in retinalthickness from baseline measured by OCT. Retinal thicknessmeasured by OCT included central thickness and the meanof the 4 inner pericentral and 4 outer quadrants separately,as described above, at 4 weeks. An ophthalmologist assessedpatients at 1 day and 4 weeks using slitlamp biomicroscopy(anterior segment and fundus).
ANTERIOR CHAMBER FLARE AFTER LASER-ASSISTED CATARACT SURGERY
salt solution (BSS Plus) fluid volume used during surgery, in-terval between the laser procedure and initiation of manualsurgery steps, postoperative IOP, and the change in retinalthickness from baseline measured by OCT. Retinal thicknessmeasured by OCT included central thickness and the meanof the 4 inner pericentral and 4 outer quadrants separately,as described above, at 4 weeks. An ophthalmologist assessedpatients at 1 day and 4 weeks using slitlamp biomicroscopy(anterior segment and fundus).